Forskel mellem versioner af "Spinal balance"
Admin (diskussion | bidrag) (→Sagittal Vertical Axis (SVA) < 3 cm) |
Admin (diskussion | bidrag) (→Pelvic Tilt (PT=PI-SS) 12º ±6 (12-18º), bør være mindre end PI/2 (ca. 26°)) |
||
| (6 mellemliggende versioner af den samme bruger vises ikke) | |||
| Linje 1: | Linje 1: | ||
| + | =Power's ratio = BC/AO < 1= | ||
| + | ved occipito-atlantal dissociation | ||
| + | |||
| + | =ADI & PADI= | ||
| + | *Atlanto-Dens Interval (ADI < 4 mm) | ||
| + | *Posterior Atlanto-Dens Interval (PADI > 14 mm) | ||
| + | |||
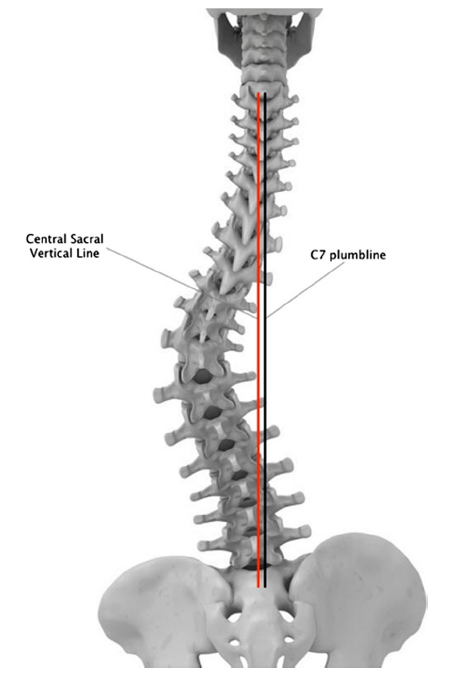
=C7 plumbline= | =C7 plumbline= | ||
| + | [[Fil:Plumbline.png]] | ||
=Sagittal Vertical Axis (SVA) < 3 cm= | =Sagittal Vertical Axis (SVA) < 3 cm= | ||
| Linje 5: | Linje 13: | ||
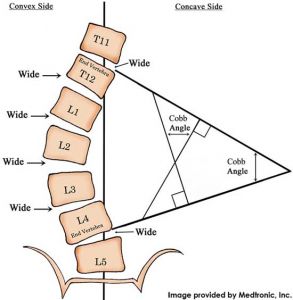
=Cobb-Lippman technique= | =Cobb-Lippman technique= | ||
| + | Skoliosen måles i coronal- eller sagittalplanet | ||
| + | |||
| + | =Vertebral rotation= | ||
| + | Vurderes med Nash/Moe metoden, se om pediklen på den ene side "forsvinder". | ||
| + | |||
| + | =Risser sign grading system= | ||
| + | Skeletal maturity | ||
| + | |||
| + | =Rib Vertebral Angle (RVA, Metha angle)= | ||
| + | Vinklen imellem en linie gennem costa og sternum, RVA-differencen < 20 = non progressive curve | ||
=Cervical Lordosis (CL) '''30º''' (20-40º)= | =Cervical Lordosis (CL) '''30º''' (20-40º)= | ||
| Linje 12: | Linje 30: | ||
Inflexion point: 46° | Inflexion point: 46° | ||
| + | |||
| + | =Cobb's angle= | ||
| + | [[Fil:Cobbangle.jpg]] | ||
| + | |||
| + | =Anterior Vertebral Body Compression (AVBC)= | ||
| + | AVBC= (V1+V3)/2 - V2 / (V1+V3)/2 | ||
=Thoracolumbar kyphosis (TLK)= | =Thoracolumbar kyphosis (TLK)= | ||
| Linje 35: | Linje 59: | ||
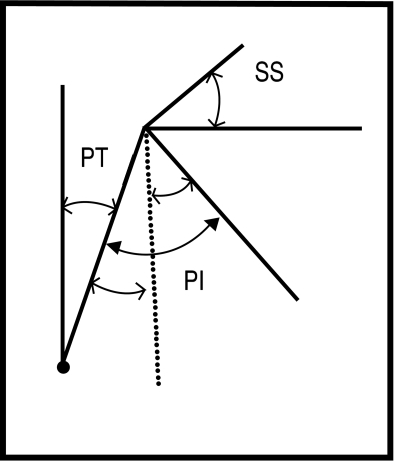
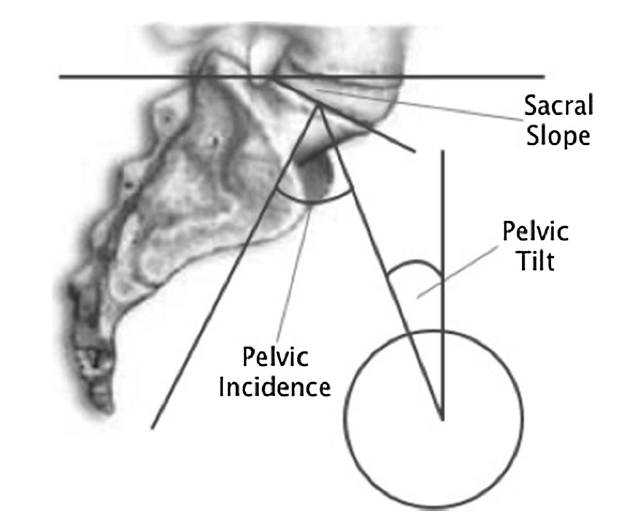
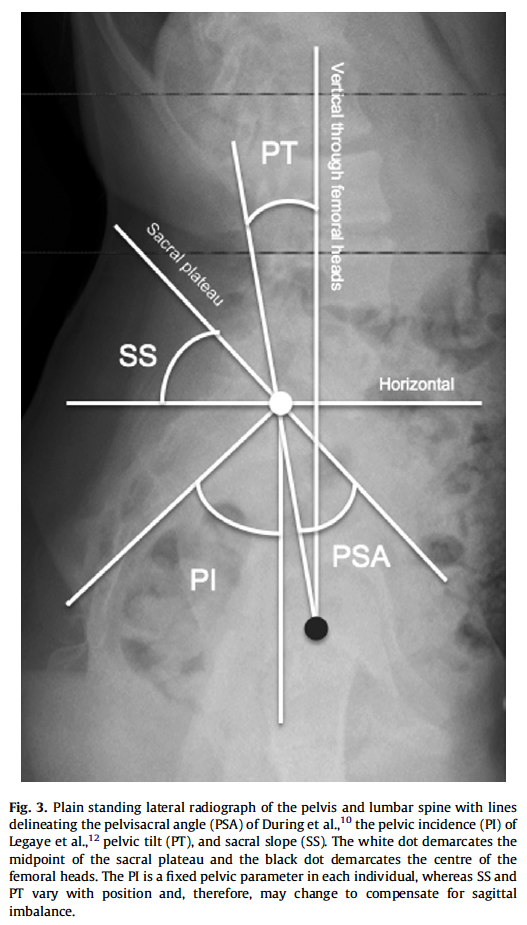
=Pelvic Incidence (PI=PT+SS) '''52º''' ±12 (48-55º)= | =Pelvic Incidence (PI=PT+SS) '''52º''' ±12 (48-55º)= | ||
Angle between the perpendicular line drawn from the center of the S1 endplate and the line that joins the center of the femoral heads to the center of the S1 endplate. PI is an angle that is '''anatomically fixed''' and is specific for each individual. This angle does not change after adolescence. High pelvic incidence (PI) increases the risk of sagittal imbalance after spine fusion and is a predictive factor for degenerative spondylolisthesis. | Angle between the perpendicular line drawn from the center of the S1 endplate and the line that joins the center of the femoral heads to the center of the S1 endplate. PI is an angle that is '''anatomically fixed''' and is specific for each individual. This angle does not change after adolescence. High pelvic incidence (PI) increases the risk of sagittal imbalance after spine fusion and is a predictive factor for degenerative spondylolisthesis. | ||
| + | *High grade PI allows maximum compensation (greater PT-range) | ||
| + | *Low grade PI don-t allow compensation (small PT-range) | ||
| + | |||
[[Fil:Relation.png]] | [[Fil:Relation.png]] | ||
| Linje 40: | Linje 67: | ||
=Pelvic Tilt (PT=PI-SS) '''12º''' ±6 (12-18º), bør være mindre end PI/2 (ca. 26°)= | =Pelvic Tilt (PT=PI-SS) '''12º''' ±6 (12-18º), bør være mindre end PI/2 (ca. 26°)= | ||
| − | Angle between the line that joins the center of the femoral heads to the center of the S1 endplate and the '''vertical line through the center of the femoral heads'''. The pelvis can rotate around the femoral heads up to a certain limit. This rotation is characterised by the pelvic tilt (PT). When the pelvis rotates backwards (retroversion), PT increases | + | Angle between the line that joins the center of the femoral heads to the center of the S1 endplate and the '''vertical line through the center of the femoral heads'''. The pelvis can rotate around the femoral heads up to a certain limit. This rotation is characterised by the pelvic tilt (PT). |
| + | *When the pelvis rotates backwards (retroversion), '''PT increases'''. PT increase with progressive kyphosis. An increase in PT after surgery is correlated with postoperative back pain. | ||
| + | *When the pelvis rotates forward (anteversion), PT decreases. | ||
| + | Restoration of a normal PT after surgery is correlated with good clinical outcome. | ||
=Sacral Slope (SS=PI-PT) '''40º''' ±9 (36-42º) bør være over PI/2 (ca. 26°)= | =Sacral Slope (SS=PI-PT) '''40º''' ±9 (36-42º) bør være over PI/2 (ca. 26°)= | ||
| Linje 46: | Linje 76: | ||
=T1 Pelvic Angle (TPA)= | =T1 Pelvic Angle (TPA)= | ||
| − | |||
| − | |||
| − | |||
=Spino-Sacral angle (SSA) 138° ±8°= | =Spino-Sacral angle (SSA) 138° ±8°= | ||
| Linje 57: | Linje 84: | ||
[[Fil:Fig3.png]] | [[Fil:Fig3.png]] | ||
| − | |||
| − | |||
[[Fil:Curvat.png]] | [[Fil:Curvat.png]] | ||
Nuværende version fra 19. okt 2014, 20:22
Indholdsfortegnelse
- 1 Power's ratio = BC/AO < 1
- 2 ADI & PADI
- 3 C7 plumbline
- 4 Sagittal Vertical Axis (SVA) < 3 cm
- 5 Cobb-Lippman technique
- 6 Vertebral rotation
- 7 Risser sign grading system
- 8 Rib Vertebral Angle (RVA, Metha angle)
- 9 Cervical Lordosis (CL) 30º (20-40º)
- 10 Thoracic Kyphosis (TK) 40º ±10º
- 11 Cobb's angle
- 12 Anterior Vertebral Body Compression (AVBC)
- 13 Thoracolumbar kyphosis (TLK)
- 14 Inflection Point
- 15 Lumbar Lordosis (LL) 50º (43-61º)
- 16 Apex L4 (L2-L5)
- 17 L5 incidence angle (L5I)
- 18 Lumbosacral angle (LSA)
- 19 Pelvic Incidence (PI=PT+SS) 52º ±12 (48-55º)
- 20 Pelvic Tilt (PT=PI-SS) 12º ±6 (12-18º), bør være mindre end PI/2 (ca. 26°)
- 21 Sacral Slope (SS=PI-PT) 40º ±9 (36-42º) bør være over PI/2 (ca. 26°)
- 22 T1 Pelvic Angle (TPA)
- 23 Spino-Sacral angle (SSA) 138° ±8°
- 24 Figurer
- 25 Lumbar instability/translation
- 26 Clinical imbalance
Power's ratio = BC/AO < 1
ved occipito-atlantal dissociation
ADI & PADI
- Atlanto-Dens Interval (ADI < 4 mm)
- Posterior Atlanto-Dens Interval (PADI > 14 mm)
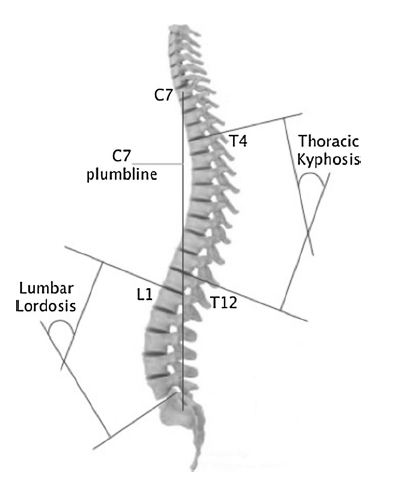
C7 plumbline
Sagittal Vertical Axis (SVA) < 3 cm
Used to evaluate the global sagittal balance. Sagittal translation of C7 plumb line. Sagittal distance between the vertical line through the center of C7 body (C7 plumbline) and the vertical line through the posterosuperior corner of the S1 endplate. An abnormal sagittal vertical axis (SVA) after fusion have a higher risk of adjacent segment degeneration.
Cobb-Lippman technique
Skoliosen måles i coronal- eller sagittalplanet
Vertebral rotation
Vurderes med Nash/Moe metoden, se om pediklen på den ene side "forsvinder".
Risser sign grading system
Skeletal maturity
Rib Vertebral Angle (RVA, Metha angle)
Vinklen imellem en linie gennem costa og sternum, RVA-differencen < 20 = non progressive curve
Cervical Lordosis (CL) 30º (20-40º)
Thoracic Kyphosis (TK) 40º ±10º
Cobb angle between the superior T1(T2-T3-T4-T5) endplate and the inferior T12 endplate.
Inflexion point: 46°
Cobb's angle
Anterior Vertebral Body Compression (AVBC)
AVBC= (V1+V3)/2 - V2 / (V1+V3)/2
Thoracolumbar kyphosis (TLK)
Cobb angle of superior endplate of T10 to inferior endplate of L2.
Inflection Point
Transition from lumbar lordosis (LL) to thoracic kyphosis (TK) is a point called the inflection point. The inflection point is not necessarily located at T12–L1, as written by anatomy textbooks, but varies according to the value of PI; its location may range from T10 to L2.
Mean: center of L1 (range: T10-L4).
Lumbar Lordosis (LL) 50º (43-61º)
Cobb angle between the superior L1 endplate and the S1 endplate. Mean value: Male 41°, Female 46° ±11°. Inflexion point: 61°
Apex L4 (L2-L5)
L5 incidence angle (L5I)
Måles som PI, bliver låst efter en fusion. Korrelation med outcome efter operation for højgrads spondylo
Lumbosacral angle (LSA)
Mellem S1- og L5-endepladen. Korrelation med outcome efter operation for højgrads spondylo
Pelvic Incidence (PI=PT+SS) 52º ±12 (48-55º)
Angle between the perpendicular line drawn from the center of the S1 endplate and the line that joins the center of the femoral heads to the center of the S1 endplate. PI is an angle that is anatomically fixed and is specific for each individual. This angle does not change after adolescence. High pelvic incidence (PI) increases the risk of sagittal imbalance after spine fusion and is a predictive factor for degenerative spondylolisthesis.
- High grade PI allows maximum compensation (greater PT-range)
- Low grade PI don-t allow compensation (small PT-range)
Pelvic Tilt (PT=PI-SS) 12º ±6 (12-18º), bør være mindre end PI/2 (ca. 26°)
Angle between the line that joins the center of the femoral heads to the center of the S1 endplate and the vertical line through the center of the femoral heads. The pelvis can rotate around the femoral heads up to a certain limit. This rotation is characterised by the pelvic tilt (PT).
- When the pelvis rotates backwards (retroversion), PT increases. PT increase with progressive kyphosis. An increase in PT after surgery is correlated with postoperative back pain.
- When the pelvis rotates forward (anteversion), PT decreases.
Restoration of a normal PT after surgery is correlated with good clinical outcome.
Sacral Slope (SS=PI-PT) 40º ±9 (36-42º) bør være over PI/2 (ca. 26°)
Angle between the horizontal and the superior S1 endplate. The sacral slope (SS) is the compensatory angle of PT and characterises the S1 endplate position. A decreased SS after fusion have a higher risk of adjacent segment degeneration.
T1 Pelvic Angle (TPA)
Spino-Sacral angle (SSA) 138° ±8°
The angle between the sacral plate and the line connecting the centroid of C7 vertebral body and the midpoint of the sacral plate.
Figurer
Lumbar instability/translation
- Skred > 4,5 mm eller hvis skreddet udgør mere end 15% af corpuslængden.
- Endepladevinkel > 22°
- Funktionsoptagelse: skred > 4,5 mm, den samlede ledskred > 15%, vinkelsum > 20° L4/L5 eller 25° L5/S1
- Meyerding grading: grad 5 (spondyloptosis: L5 ligger under S1)
Clinical imbalance
Three types of disturbances may arise, leading to a displacement of the trunk forwards and inducing an sagittal unbalance with excessive stresses of the anatomical structures and necessitating muscle contractions, possibly painful:
Type A
Lack of “Lordosis” with a “Sacral Slope” value too low for the value of PI; (Figure 7) It was the most frequently observed disturbance in clinical practice for low back pain. The loss of “Lordosis” was the consequence of lumbar disorders, mostly at the lower levels (disc diseases with local inter vertebral reduction of the lordosis, fractures …), the result of fusion in inadequate lordosis or the result of muscular atrophy (often with obesity, sometimes by muscular or neurological disorders s as Parkinson’s disease). The pelvic reaction to this loss of lordosis was a backward rotation (retroversion) achievable by extension of the hips, and then by flexion of the knees (and flexion of he ankles).
Type B
Excessive “Sacral Slope” value reflecting a forward pelvic rotation (anteversion), by stiff flexion of the hips, sufficiently or not compensated by an accentuation of the “Lordosis”. (Figure 7) This situation occurred mostly in cases of hip (and knee) osteoarthritis. Only the treatment of the origin was useful (as by hip arthroplasty).
Type C
"Lordosis” insufficient to compensate an excessive kyphosis, with backwards pelvic rotation (low value of SS), and finally flexion of the hips and the knees. (Figure 7) This situation occurred mostly with aging, by disc thoracic narrowing or osteoporotic factures, after traumatic fractures or in majors Scheuerman’s diseases cases.