Spinal Stenosis
Indholdsfortegnelse
- 1 Overview
- 2 Anatomy
- 3 Disc
- 4 Facet Joints
- 5 Intervertebral Foramen
- 6 Cauda Equina
- 7 Classification
- 8 Deformity and Instability
- 9 Pathophysiology
- 10 Natural History
- 11 Clinical Presentation
- 12 Physical Examination
- 13 Diagnostic Studies
- 14 Magnetic Resonance Imaging
- 15 Electromyography, Nerve Condition Studies, and Somatosensory Evoked Potentials
- 16 Differential Diagnosis
- 17 Summary
- 18 Pearls
- 19 Pitfalls
- 20 Key Points
- 21 Key References
Overview
Spinal stenosis is one of the most common conditions in the elderly. It is defined as a narrowing of the spinal canal. The term stenosis is derived from the Greek word for narrow, which is "stenos." The first description of this condition is attributed to Antoine Portal in 1803. Verbiest is credited with coining the term spinal stenosis and the associated narrowing of the spinal canal as its potential cause. Kirkaldy-Willis subsequently described the degenerative cascade in the lumbar spine as the cause for the altered anatomy and pathophysiology in spinal stenosis.
Narrowing in the spine can occur in the central canal, lateral recess, or foramen, leading to compression of the neural elements in those locations. The symptoms produced vary by the location of the neural compression. Neural compression in the central canal leads to the commonly seen clinical presentation of low back pain radiating into bilateral legs. Patients typically also describe heaviness and weakness in their legs that worsens with ambulation and improves with leaning forward or resting. Degeneration of the spine with aging leads to alteration in the anatomy causing gradually progressive narrowing of the spinal canal.
The term spinal stenosis refers to an anatomic diagnosis that increases with age and can occur in asymptomatic individuals. The exact reason for why some with this condition have debilitating symptoms while others have no symptoms is not well understood. These differences in presentation may be related to the different abilities of individuals to compensate for the anatomic changes that have occurred. When symptoms do present, they usually occur on the basis of the location of neural compression. Patients with central canal stenosis typically present with neurogenic claudication, whereas those with lateral recess and foraminal stenosis present with radicular pain. Patients with significant symptoms that do not respond to conservative treatment often elect surgical treatment. In fact, in adults older than 65, spinal stenosis is the most common reason to undergo lumbar spine surgery.
Anatomy
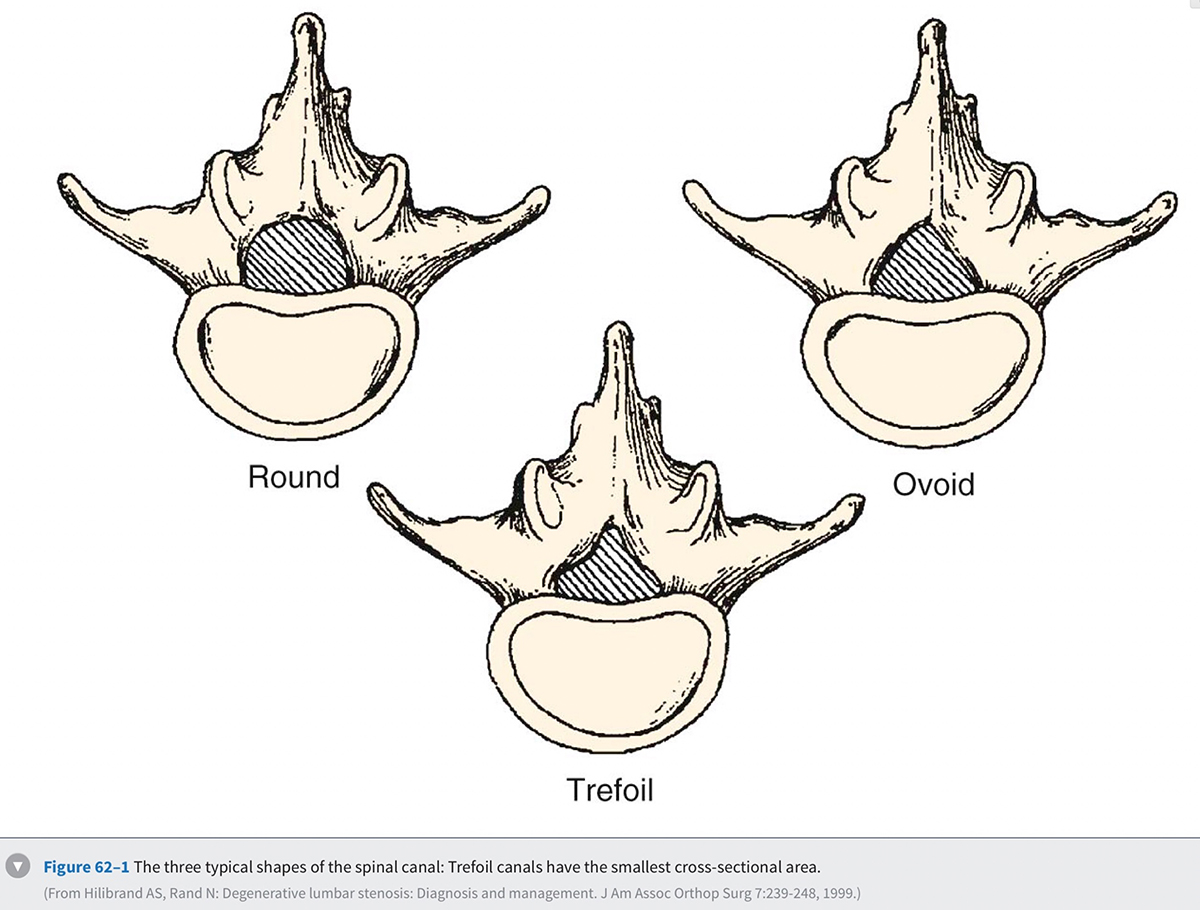
In order to understand how spinal stenosis causes symptoms, we must first have a good understanding of the normal anatomy of the lumbar spine. The spinal canal's anterior border is formed by the vertebral body, the disc, and the posterior longitudinal ligament. The lateral border is formed by the pedicles, the lateral ligamentum flavum, and the neural foramen. The posterior border is formed by the facet joints, lamina, and ligamentum flavum. The shape of the spinal canal may be circular, oval, or trefoil (Fig. 62-1 ). The circular and oval canal shapes provide the most space for the neural elements centrally and in the lateral recess. The trefoil canal has the smallest cross-sectional area. It is present in 15% of the individuals and predisposes these individuals to lateral recess stenosis.
Disc
Disc degeneration is believed to be the first step in degeneration of the spine. At birth, the nucleus pulposus and the annulus occupy roughly 50% of the disc area. The nucleus is gelatinous and there is a discrete boundary between the nucleus and the annulus. Over time the collagen content increases and the demarcation between the nucleus and the annulus becomes less distinct. Other structures within the disc also change with aging. The chondroitin sulfate concentration decreases, and the ratio of keratin sulfate to chondroitin sulfate increases. Because keratin sulfate has less hydrophilic potential, the disc dehydrates over time.
Hydration of the disc also changes due to an alteration in the type of collagen within the disc over time. The annulus contains 60% type II and 40% type I collagen, whereas the disc contains mainly type II collagen. Type I collagen is associated with decreased water content compared with type II collagen. Thus as the type I collagen content increases with age, hydration of the disc decreases. The normal nucleus pulposus typically consists of 85% water, whereas the annulus consists of 78% water. With degeneration of the disc, the water content drops to roughly 70%. A desiccated disc has a decreased ability to handle mechanical load.
The Kirkaldy-Willis theory explains how these changes progress over time. This theory is based on viewing the spine as a tripod with the disc and the two facet joints making up the three legs. This analogy makes it easier to understand how alteration in one joint can alter the others. The initial stage in the degenerative cascade is circumferential tearing of the annulus, which progresses to radial tears. This, along with the biochemical changes in the disc described previously, leads to further degeneration of the disc and disc height loss. Altered disc structure and disc height loss lead to bulging of the disc and the posterior longitudinal ligament. This causes narrowing of the spinal canal and potential neural impingement. The lost disc height also leads to buckling of the ligamentum flavum and settling of the facet joints. The facet joints subsequently deteriorate and form osteophytes, which further narrows the spinal canal. The altered structure, motion, and biomechanics then lead to additional disc deterioration, which propagates the cycle of degeneration.
Facet Joints
The lumbar facet joints are encapsulated structures that have a uniform cartilaginous surface to produce a smooth gliding motion. The superior articular process is concave and its articular surface faces medially and dorsally. The inferior articular process is convex and its articular surface faces laterally and ventrally. Lumbar facet joints are oriented 90 degrees in the sagittal plane and 45 degrees anterior in the coronal plane. Studies show that more sagittally oriented facet joints are associated with a degenerative spondylolisthesis. The two facet joints are usually symmetric with respect to their joint angles at each level. Facet tropism refers to an asymmetry between the facet joints and has been theorized to lead to degeneration.
As the disc degenerates and narrows, the facet joints settle and increased stress is placed across the facet joint. This leads to facet joint degeneration, hypertrophy, and osteophyte formation. These osteophytes can cause impingement of the thecal sac within the spinal canal or the nerve root in the neural foramen.
Intervertebral Foramen
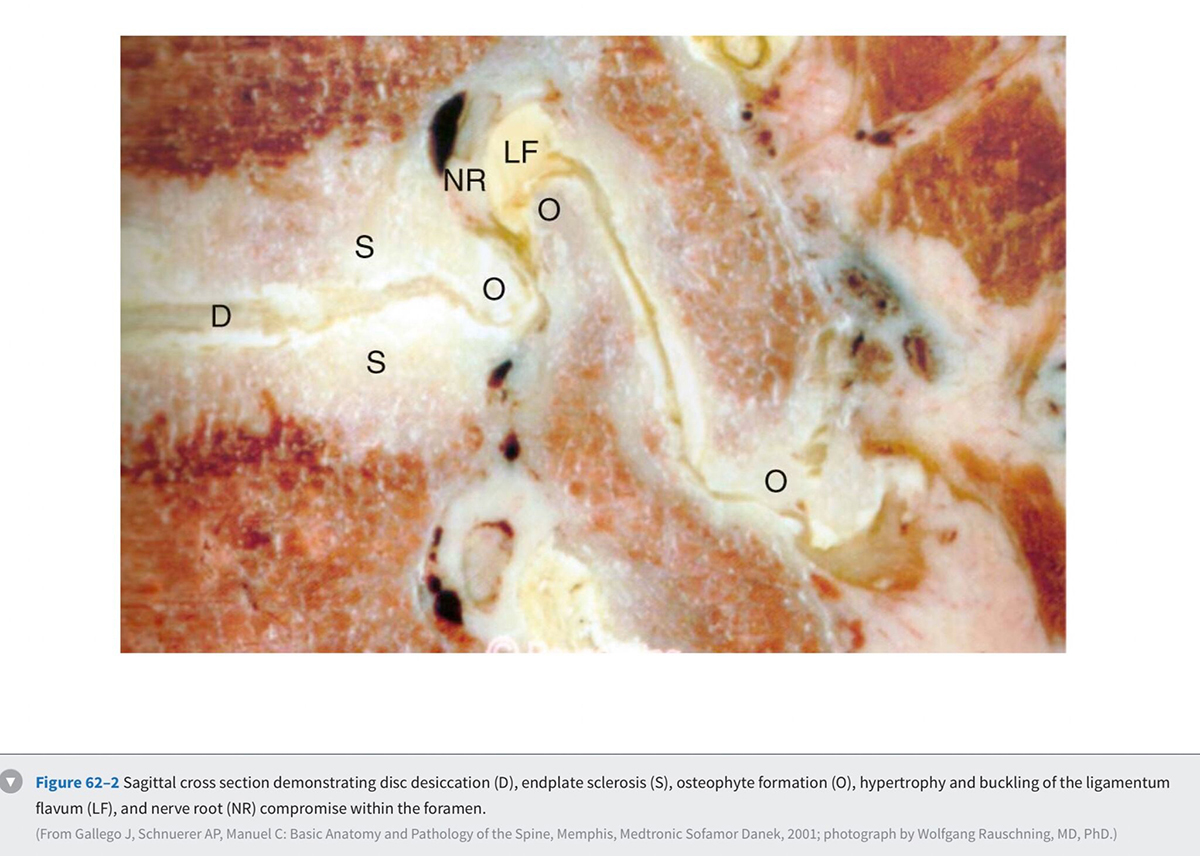
The anterior boundary of the intervertebral foramen is made up of the posterior wall of the vertebral body and the disc. The posterior boundary is made up of the lateral aspect of the facet joint and the ligamentum flavum. Superior and inferior boundaries are formed by the pedicles of the vertebral bodies corresponding to that segment. The foramen is typically larger than the ganglion and the nerve that it contains. The additional space is occupied by fat and loose areolar tissue that can accommodate for motion. With degeneration, hypertrophy of the facets can cause posterior compression of the neural elements (Fig. 62-2) . Anterior compression of the neural elements usually arises from endplate osteophytes or foraminal disc herniations. Decrease in disc height with degeneration can cause a decrease in the foraminal height and neural compression. This type of vertical or up-down foraminal stenosis is important to recognize because a posterior decompression alone may not significantly improve the vertical compression and may result in persistent symptoms after surgery.
Cauda Equina
The thecal sac lies in the spinal canal and gives rise to nerve roots at each segment. The nerve root initially courses along the medial aspect of the pedicle and then progresses laterally, inferior to the pedicle in the neural foramen. The nerve roots within the cauda equina are arranged in a predictable pattern within the thecal sac (Fig. 62-3). Cross section of the thecal sac demonstrates the most caudal roots to be present in a central and posterior position. The more cephalad roots are located sequentially more lateral and anterior. At each level, the motor fibers of a root are anterior and medial to the larger sensory component. Dorsal root ganglia exist at every level and can be intraspinal or intraforaminal. A variety of clinical presentations arise on the basis of the anatomic location of neural compression.
Classification
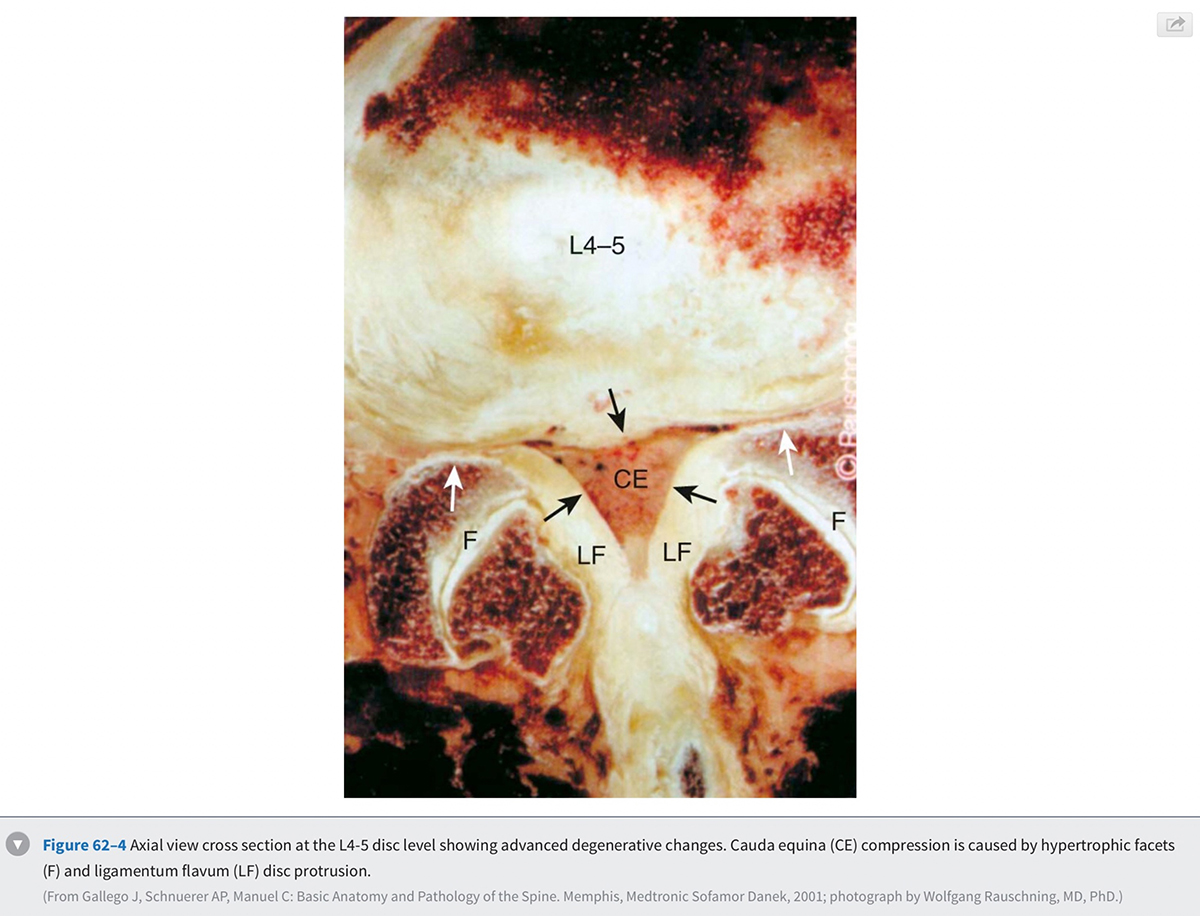
Stenosis can be anatomically classified as central, lateral recess, and foraminal on the basis of the location of neural compression. With aging, central canal stenosis occurs as degenerative changes progress. As the axial height of the disc and facet joints decreases, the disc bulges into the spinal canal. The central canal is further narrowed by posterior impingement from enlarged facets and the hypertrophied ligamentum flavum (Fig. 62-4). Hypertrophy of the soft tissues is responsible for 40% of spinal stenosis. With extension, the hypertrophied ligamentum buckles centrally into the canal and worsens the central stenosis. This explains why patients with stenosis typically report worsening of their symptoms in extension.
Lateral recess stenosis typically results from posterior disc protrusion in combination with some superior articular facet hypertrophy. Lateral recess stenosis can present with lumbar radiculopathy, and incidence of lateral recess stenosis ranges from 8% to 11%. These patients present with pain or neurologic symptoms in a dermatomal distribution on the basis of the nerve that is compressed in the lateral recess.
Foraminal stenosis causes compression of the exiting nerve root and ganglion and also leads to lumbar radiculopathy. Foraminal stenosis occurs most commonly in the lower lumbar spine with the fifth lumbar nerve root being the most commonly involved. Foraminal stenosis can occur from loss of disc height, vertebral endplate osteophytes, facet osteophytes, spondylolisthesis, and disc herniations. Like central canal stenosis, foraminal stenosis is worse in extension and thus exacerbating and alleviating factors for symptoms from foraminal compression are similar to those from central canal stenosis.
Spinal stenosis can also be classified on the basis of the etiology, which can be congenital, acquired, or both. Congenital stenosis is present as a normal variant in the population and is part of certain conditions such as dwarfism. In these conditions, patients have short pedicles that are closer together than the normal lumbar spine. In congenital stenosis, few degenerative changes are sufficient to cause neural compression and symptoms. As one would expect, congenital stenosis becomes symptomatic much earlier in life and patients usually become symptomatic in the fourth decade. Acquired stenosis can be caused by trauma, neoplasms, and infection, along with other causes listed in Box 62-1.
BOX 62-1 Classification of spinal stenosis
- Congenital/developmental
- Idiopathic
- Achondroplastic
- Osteopetrosis
- Acquired
- Degenerative
- Central
- Lateral recess
- Foraminal
- latrogenic
- Postlaminectomy
- Adjacent to fusion
- Malposition of hardware in the canal
- Post-procedure epidural hematoma
- Miscellaneous disorders
- Acromegaly
- Paget's
- Fluorosis
- Ankylosingspondylitis
- Traumatic
- Degenerative
- Combined
Any combination of congenital/developmental or acquired stenosis
Deformity and Instability
The static changes that we discussed thus far can be worsened by dynamic factors such as segmental instability. Instability typically arises from degenerative changes and can be in the form of translational or rotational abnormality. Translational abnormality is found most commonly in women as a degenerative anterolisthesis of L4 on L5. The attachment of the iliolumbar ligaments to the L5 level may act as a restraining force and cause more relative motion at L4-5. The more sagittally oriented facet joints between the fourth and fifth lumbar vertebrae can be an additional predisposing factor for instability at this level. Because the lamina and the spinous process typically project inferior to the vertebral body, the amount of room available between the inferior aspect of the L4 lamina and the posterior superior aspect of L5 is substantially decreased. This anterior translation of the L4 posterior elements, along with hypertrophy of the facets and the ligamentum flavum, leads to central and lateral recess stenosis. Foraminal stenosis can also occur in this setting with collapse of the disc space, disc herniation, endplate osteophytes, or facet hypertrophy. With scoliosis, lateral subluxation and rotational instability can cause altered biomechanics that leads to degeneration. The altered anatomy can also be a cause of narrowing of the central canal, lateral recess, and foraminal regions. Degenerative changes superimposed on abnormal anatomy lead to stenosis in these patients.
Pathophysiology
The term spinal stenosis describes the anatomic narrowing of the spinal canal. How does spinal stenosis result in pain and altered neurologic function? A number of cadaver and animal studies have attempted to elucidate the mechanism of these symptoms. Schonstorm evaluated the changes in nerve pressure that occur as the spinal canal narrows. In his human cadaver study, the thecal sac constriction of 45% or more led to an increased pressure in the nerve roots. As the degree of compression increased, the pressure in the nerve roots increased. Delamarter and colleagues also demonstrated the importance of the magnitude of thecal sac compression in alteration of neural function. They noted no alteration in neurologic function when the animal's cauda equina was constricted by 25%, whereas more than 50% compression led to motor or sensory deficits. Pedowitz and colleagues demonstrated that the duration of compression was also an important factor in neural dysfunction.
Rydevik and colleagues demonstrated another effect of compression of the thecal sac. They noted that once pressure of more than 50 mm Hg was achieved, capillary restriction and electrophysiologic alteration occurred in the nerve roots. Even at pressures as low as 5 to 10 mm Hg, venous congestion of the intraneural microcirculation occurred. Solute transport decreased 45% across nerve root segments with the low pressure of 10 mm Hg. This suggests that low-grade sustained compression of the nerve roots could lead to vascular impairment and potential detrimental changes in the function of the nerve roots. In addition to neural compression and altered nutrition, inflammatory chemical mediators have also been shown to be a cause of pain.
The presence of stenosis increases with aging; however, it often does not produce any symptoms. What causes pain in some individual with mild spinal stenosis and no symptoms in others with severe stenosis? The experimental evidence reviewed earlier suggests that each individual may have an innate ability to compensate for the accumulating pathologic changes. Because the magnitude an individual can compensate for is different for different people, two individuals with the same amount of stenosis may not exhibit the same symptoms. The rate at which these changes are occurring also appears to be important. Individuals may become symptomatic with a lower magnitude of compression if it occurs rapidly. This explains how a patient with stenosis can become symptomatic with an acute mild disc herniation.
Natural History
Patients with congenital stenosis typically become symptomatic earlier in life. Due to congenital narrowing of the canal in these patients, significant stenosis is present at multiple levels even with little degenerative change. Patients with degenerative stenosis present later in life during their 60s and have far more advanced degeneration in their spine. Females are more commonly affected with stenosis and the L4-5 level is the most common segment involved.
Multiple studies have looked at the short-term and long-term results of nonoperative treatment of patients with lumbar stenosis. These studies show that a significant number of patients respond favorably to nonoperative treatment. Some patients, however, do not improve and some even worsen. Johnsson and colleagues reviewed the results of 32 patients who declined to have surgery at a 4-year follow-up period. They noted that 70% of patients were unchanged, while 15% were the same and 15% worsened.
Recently, prospective studies have reported short-term and long-term results of nonoperative and operative treatment. The Maine Lumbar Spine prospective observational study reported 8- to 10-year follow-up results on 97 patients. They noted that a large number of patients (39%) that had initially elected nonsurgical treatment subsequently elected to undergo surgery. Of the patients who continued nonoperative treatment, most had stable symptoms. Miyamoto and colleagues reported prospective results of nonsurgical treatment in 120 patients. Sixteen percent of the patients required surgical treatment during the follow-up period of 5 years. Of the nonsurgically treated patients, 53% of patients reported no hindrance during the activities of daily living. No sudden neurologic deterioration was reported. Roughly 23% of patients had worsened but did not elect to undergo surgical intervention.
The Finnish Lumbar Spinal Research Group reported the results of a randomized controlled trial in 2007. They randomized 94 patients with mild to moderate stenosis into either the surgical group or nonoperative group. At the 2-year follow-up, patients noted improvement of symptoms in both groups; however, the outcome of patients undergoing surgical treatment was significantly better. The most recent prospective study to evaluate patients with lumbar stenosis is the SPORT study. This study reported prospective outcomes of 634 patients at 2-year follow-up. Patients undergoing surgical treatment had better outcomes than those who underwent nonsurgical treatment. Patients in the nonsurgical treatment group showed small improvements in most outcome measures. It should be noted that no disastrous neurologic deterioration was noted with nonoperative treatment.
The recently published North American Spine Society evidence-based guidelines for diagnosis and treatment of lumbar stenosis provide some tangible conclusions from these studies. They state that in one third to one half of patients with mild to moderate stenosis, the natural history is favorable. Unfortunately, predicting which patients with stenosis will worsen over time is impossible. In some studies symptomatic patients with severe stenosis did poorly over time, but overall there is not sufficient evidence to draw any conclusions. What is known is that rapid or catastrophic deterioration is rare in patients with spinal stenosis. Knowing this can be helpful in guiding treatment and evaluating these patients. When a patient with spinal stenosis has rapidly worsening neurologic status, other causes of neurologic dysfunction should be investigated.
Clinical Presentation
Patients with lumbar spinal stenosis most commonly present with leg pain. This leg pain presents as either neurogenic claudication or radicular leg pain. Patients with neurogenic claudication report a feeling of pain, heaviness, numbness, cramping, burning, or weakness. The symptoms typically start from the back or the buttocks and bilaterally radiate down below the knees. One lower extremity may be worse than the other; however, both legs are typically involved. Symptoms usually do not follow a dermatomal pattern and are usually related to activities. These abnormal sensations are typically worse with extension of the lumbar spine during walking or standing for a prolonged time. Some report worsening weakness if they keep walking. They may note ankle dorsiflexion weakness that is typically described as feet slapping or even falling as they attempt to keep walking. Walking downhill is more challenging for these patients as the lumbar spine is extended while going downhill. Most describe a set distance they can walk before the symptoms become disabling. As the stenosis worsens, this distance typically decreases, further disrupting the daily life and function of these patients. Relief of symptoms typically comes from flexing the lumbar spine by leaning forward, sitting, or lying down. As discussed earlier, the degree of stenosis decreases as the lumbar spine is flexed and patients naturally learn to position themselves in a posture that minimizes discomfort and maximizes function. Keeping this in mind, it is easy to understand why these patients typically lean forward on a grocery cart and have an easier time riding a bike, walking uphill, or driving while sitting in a car.
In contrast to neurogenic claudication arising from compression of the thecal sac, radicular pain arises from compression of a particular nerve root in the lateral recess or the neural foramen. Unlike claudication, radicular leg pain is described by the patients in a specific dermatomal pattern corresponding to the compressed nerve root. The most common presentation of this is L5 radiculopathy from lateral recess stenosis causing compression of the L5 nerve root. In addition to numbness in the L5 distribution, weakness can be seen in extensor hallucis longus and tibialis anterior muscle groups.
Low back pain is also a common complaint in patients with stenosis. Although most patients note the radiation of this pain into their legs, some present without leg pain or note radiation of the pain only into their buttocks. Exacerbating and alleviating factors for claudicatory low back pain are similar to those for the leg pain. Spondylotic change with or without spondylolisthesis is a common finding in this patient population and often the cause for low back pain. Patients with symptoms in both the low back and leg have a greater disability than those who have symptoms only in one location.
Severe neurologic symptoms such as bowel and bladder incontinence or profound weakness are uncommon in patients with stenosis. Urinary dysfunction is a common complaint in this elderly population and can be present in 50% to 80% of patients.61'62 Because various causes of urinary dysfunction such as preexisting stress incontinence, urinary tract infections, and prostatic hypertrophy are common in this population, a careful history can help exclude these common causes. The factors more commonly noted in patients with neurogenic bladder dysfunction are perianal sensory disturbance, longer duration of symptoms, and higher mean residual volumes on urodynamic studies.
In addition to obtaining a history specific to the patient's pain and neurologic symptoms, it is important to obtain a comprehensive medical history. A patient's report of preexisting peripheral arterial occlusive disease, hip arthritis, multiple sclerosis, or neuropathy would substantially alter what symptoms are attributed to the stenosis. Similarly, obtaining an overall picture of the medical comorbidities and physiologic condition will also shed light on the ability of the patient to safely undergo any invasive procedures. Knowing the patient's other medical conditions can also help identify patients who may be at risk for inferior outcomes. Cardiovascular comorbidities, depression, and disorders influencing walking ability have all been noted to be preoperative predictors of poor postoperative outcomes.
Physical Examination
A good physical examination of patients with lumbar spinal stenosis should start with observation. Often these patients will be sitting flexed forward on a chair in the examination room. While standing and ambulating, stenosis patients still often flex their trunk forward to decrease their symptoms. This may also be noticed when checking their range of motion as a decrease in the active lumbar extension. Reproduction of the patient's usual symptoms by prolonged lumbar extension can also be helpful in confirming the diagnosis. Neurologic examination is often normal in spite of long-standing debilitating symptoms. Lateral recess stenosis is more commonly responsible for neurologic changes.65 When motor weakness or sensory deficit is present, it is most often in the L5 distribution. A frequent neurologic finding is an asymmetrical deep tendon reflex at the patellar or Achilles tendon. A symmetric decrease in the reflexes is more indicative of age-related changes. Nerve root tension signs are usually not present. Changes in neurologic examination may become more obvious after stressing the patient's neurologic system. This can be accomplished by asking the patient to walk until he or she experiences significant symptoms. Re-examination at this point may reveal changes in motor, sensory, or reflex examination that were not detected before the stress.
It is useful to review physical examination findings found in some studies to get a better idea of their frequency. Amundsen and colleagues66 prospectively evaluated the clinical and radiographic features of 100 patients with symptomatic spinal stenosis. They reported a motor weakness in 23% and sensory deficit in 51%. In the 2007 randomized controlled trial of 94 stenosis patients from the Finnish Lumbar Spinal Research Group, 22% of patients had an L5 motor weakness and 19% had a sensory deficit. Straight leg raise test was positive in 3% of the patients. In the recent SPORT study, asymmetric reflexes were noted in 26%, motor weakness was noted in 28%, and sensory deficit was noted in 29%.
An important part of the physical examination must be identifying other common causes of similar symptoms. The neurologic examination should focus on eliciting signs that would suggest other neurologic causes of the patient's symptoms. Hyper-reflexia, clonus, and upgoing toes, along with other upper motor neuron findings, can suggest the presence of myelopathy from cord compression. Sensory disturbance in a stocking distribution suggests the presence of neuropathy. A general musculoskeletal examination must include assessing the irritaimity anu limitation of motion in the nips to rule out nip pathology. Palpation of the greater trochanter and iliotibial band can help detect pathology in these easily treated structures. Diminished peripheral pulses along with diminished skin hair are important clues that the symptoms may be coming from vascular claudication.
Diagnostic Studies
Radiography
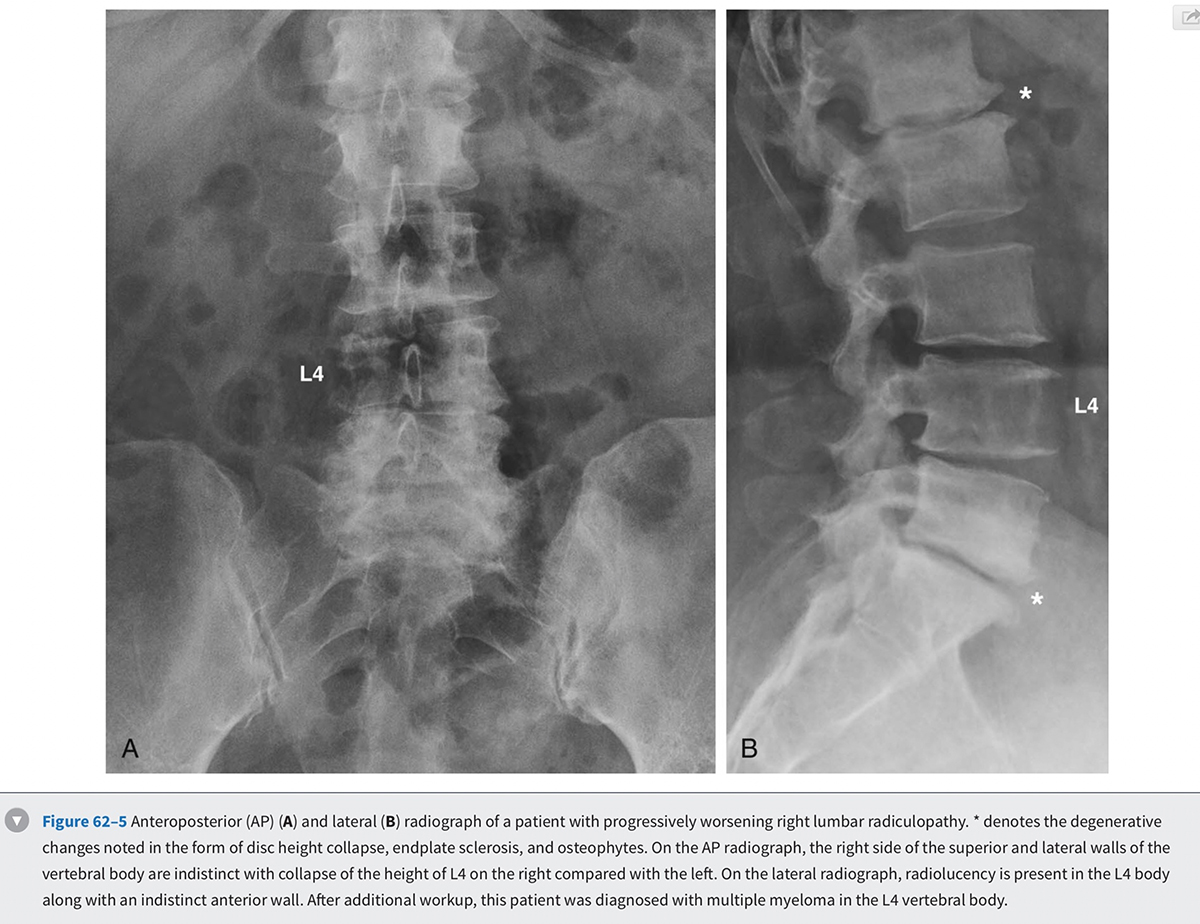
The diagnostic testing of patients with spinal stenosis often starts with plain radiographs. In addition to the anteroposterior and lateral radiographs, flexion and extension lateral views should be considered. Most patients suspected of stenosis are elderly and thus likely demonstrate a variety of spondylotic changes on the radiographs. Particular attention should be paid to diagnosing scoliosis and spondylolisthesis in addition to any dynamic instability that can be detected on the flexion-extension views. If scoliosis is noted, long cassette scoliosis films would be helpful in evaluating the full extent of the deformity in both the coronal and sagittal planes. Narrowing of the neural foramen and inferred narrowing of the spinal canal from the location and extent of degenerated structures should be evaluated. Ossification of ligamentous structures, ankylosis of the spine, erosion of the disc space, or any abnormal appearance of the bony structures should be assessed (Fig. 62-5 0 ). It should be kept in mind that even severe degenerative changes can be seen in asymptomatic patients.
Computed Tomography with and Without Myelography
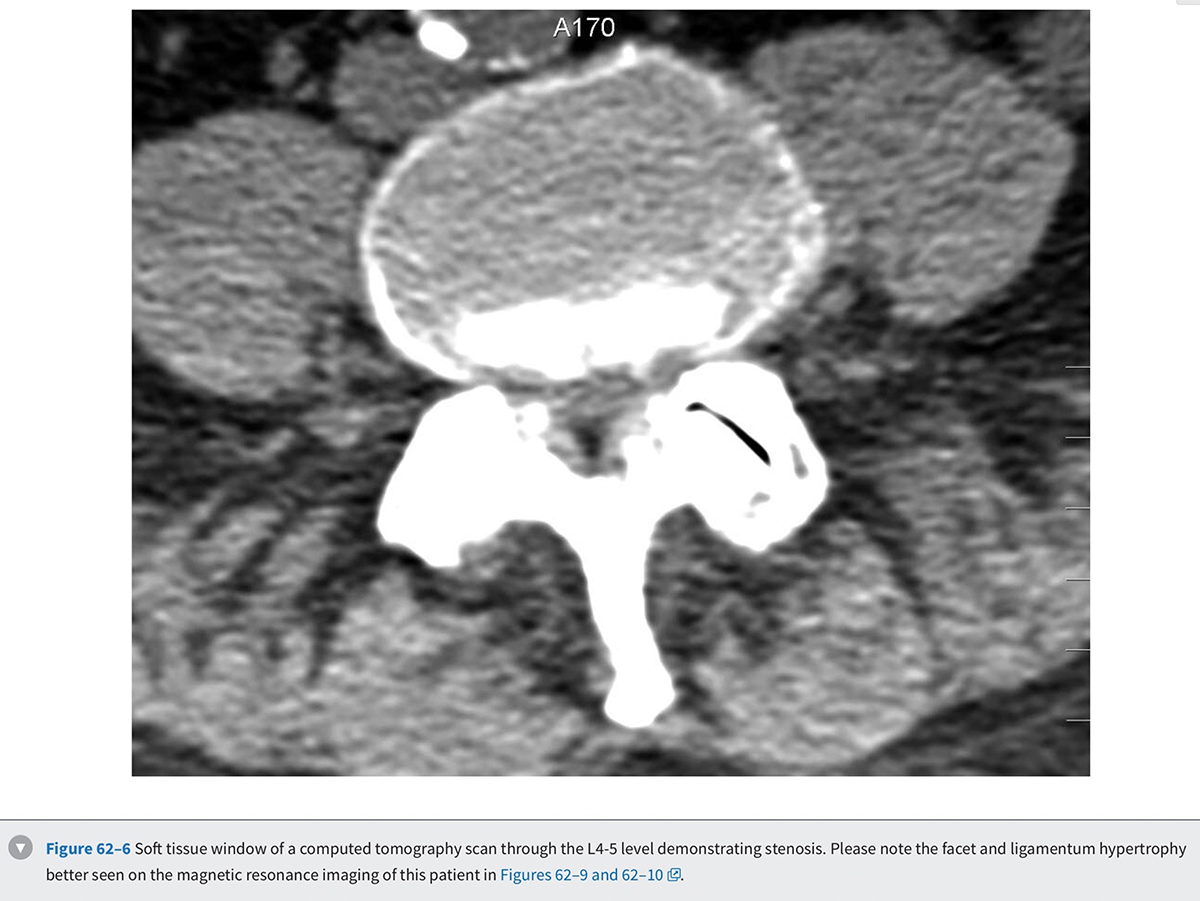
Prior to the common availability of magnetic resonance imaging (MRI), a computed tomography (CT) scan was the study of choice for visualizing pathologic anatomy in the axial plane. Because a significant portion of the stenosis comes from soft tissue pathology, visualization of the soft tissues is the top priority in axial imaging. A CT scan is a poor modality for detailed analysis of the soft tissue pathology (Fig. 62-6 g ). A meta-analysis demonstrated that the sensitivity of a CT scan in detecting spinal stenosis ranges from 70% to 100%.
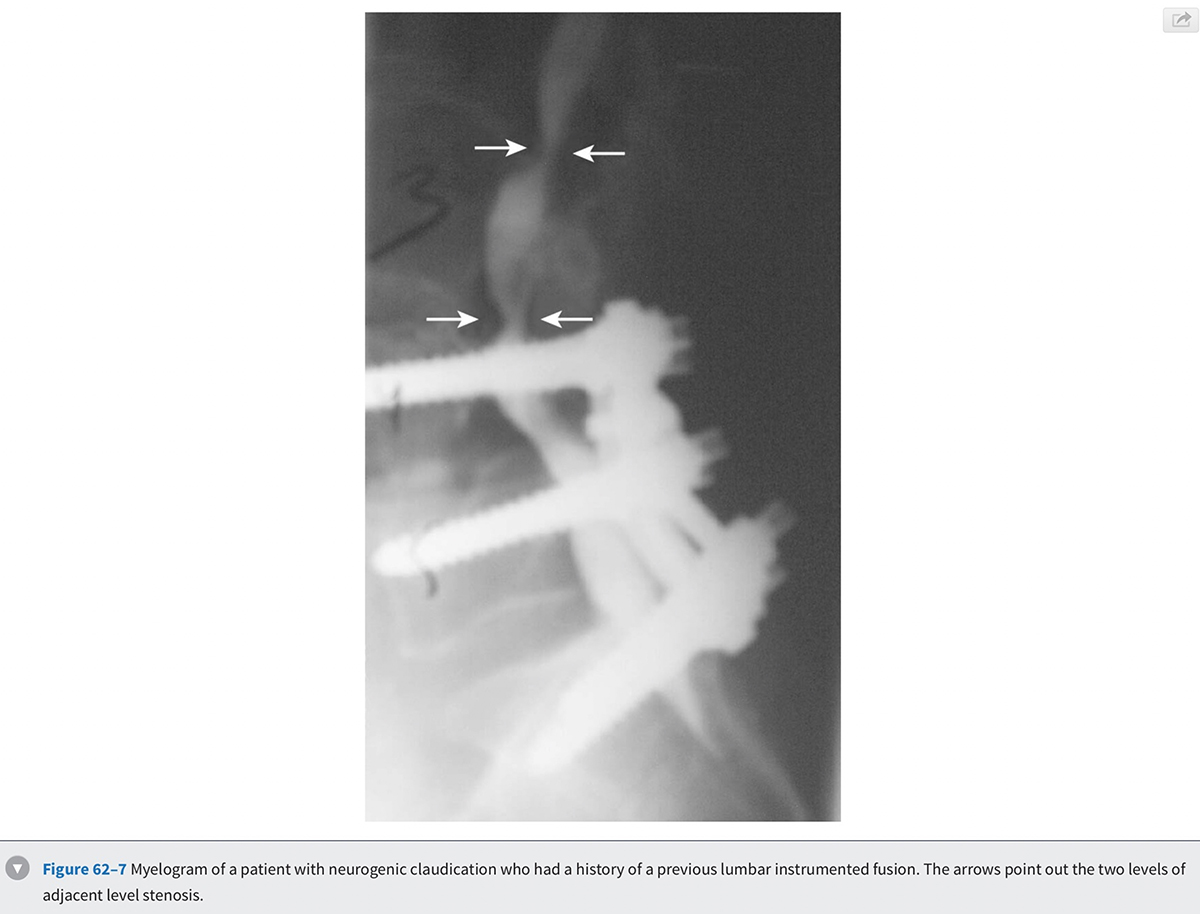
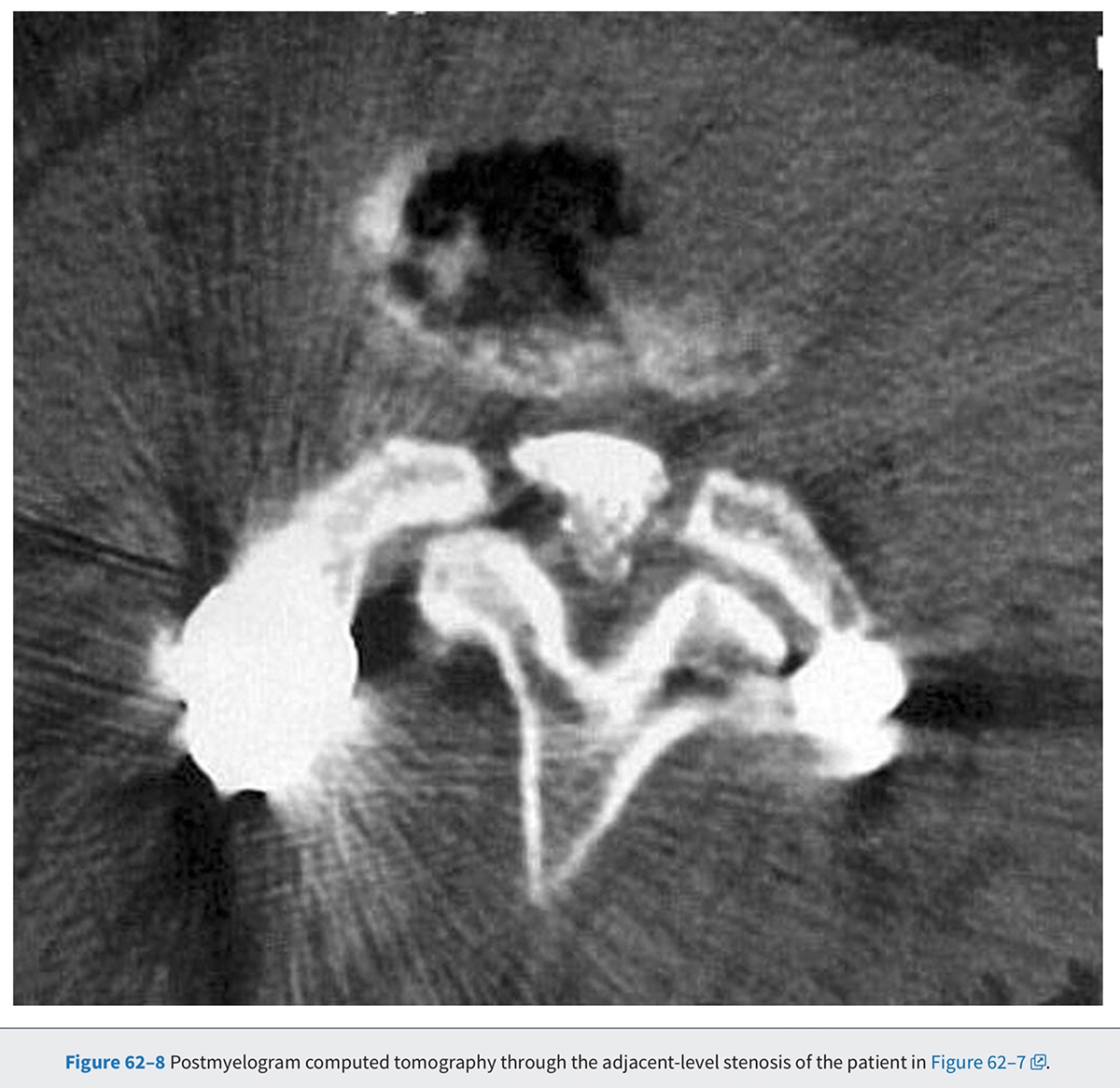
Diagnostic utility of the CT scan can be improved by combining it with myelography. The dye injected in the cerebrospinal fluid (CSF) during a myelogram provides good contrast between the thecal sac and the surrounding soft tissue and bony pathology. Preoperative complete contrast block on a CT-myelogram has been correlated with an improved surgical outcome.' The invasiveness of the myelogram and the radiation associated with the CT are the two biggest drawbacks of this diagnostic modality. Given these limitations, patients who are unable to have an MRI, who have scoliosis, or who have previous spinal instrumentation are the most likely to undergo this study (Figs. 62-7 and 62-8). In cases where MRI findings are unclear, a CT or a CT-myelogram should be considered to gain further information about the pathology.
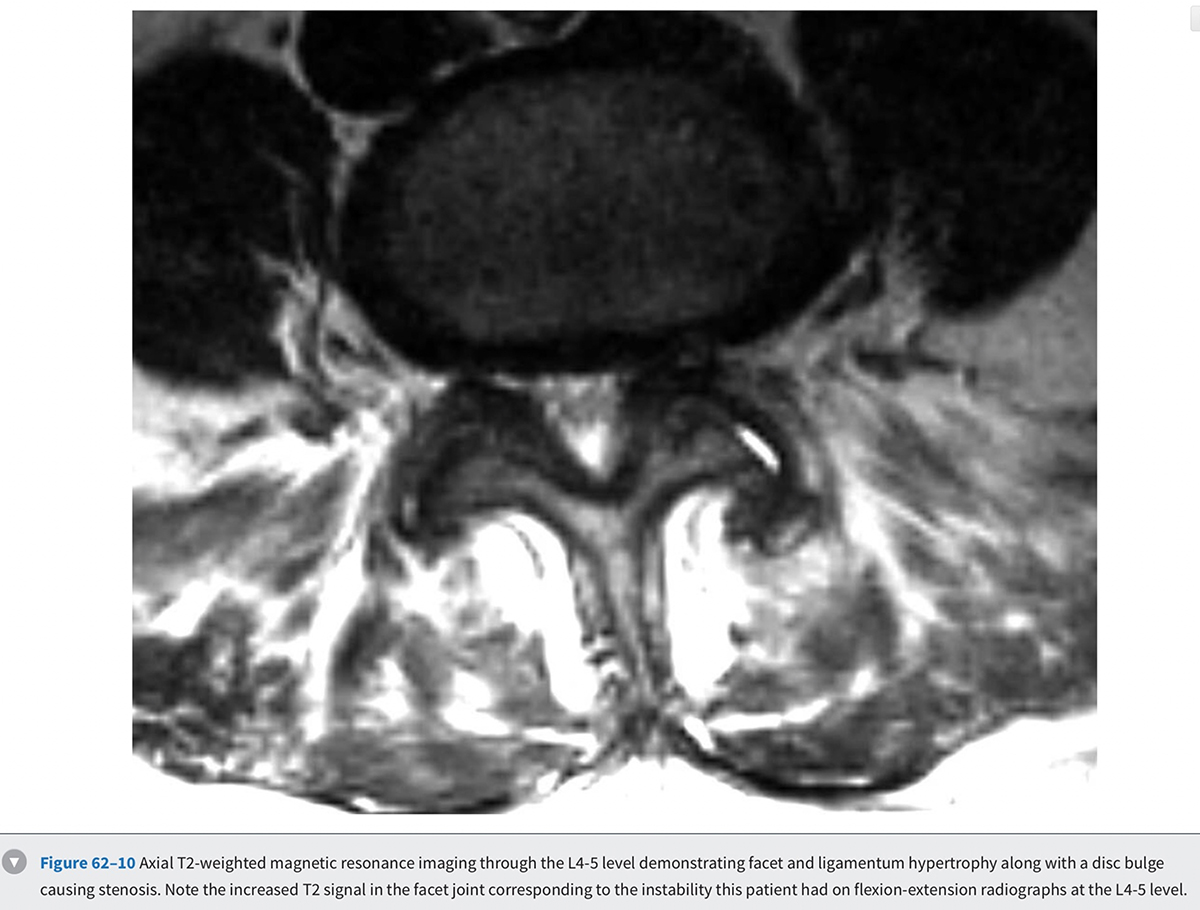
Magnetic Resonance Imaging
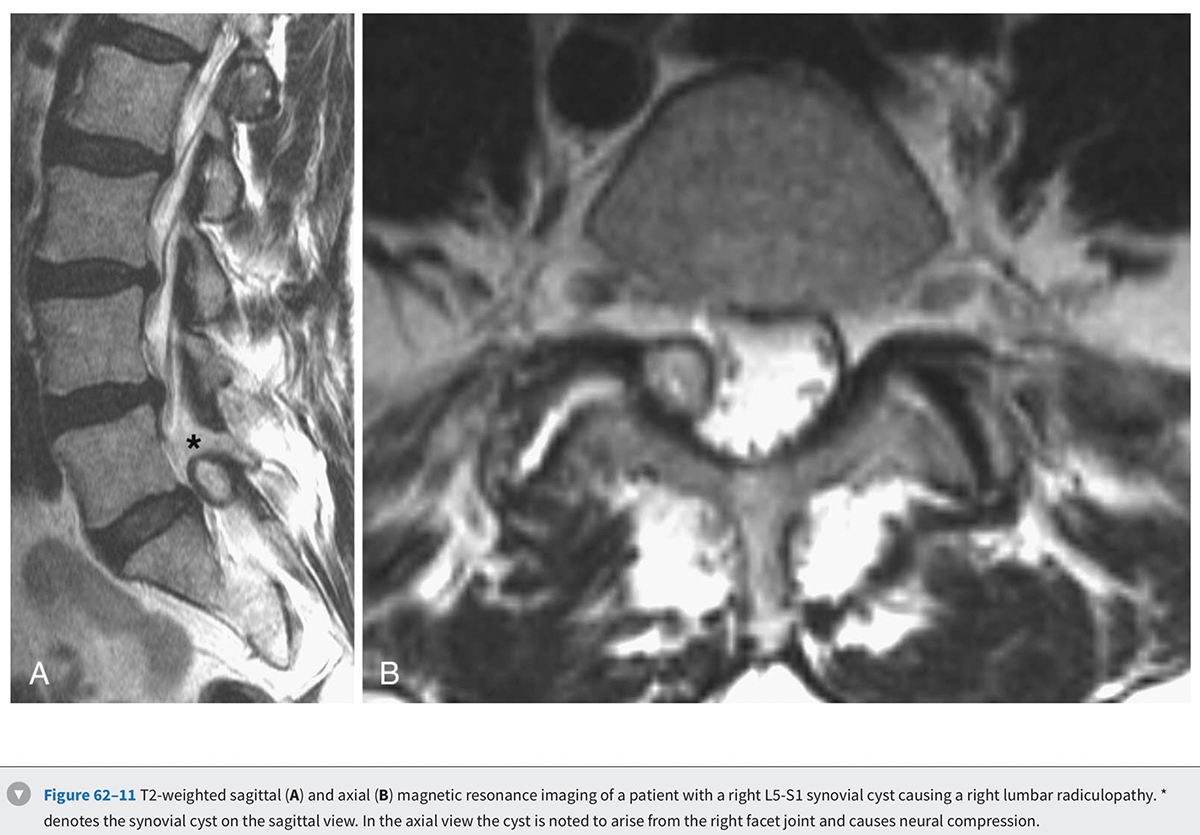
MRI is the diagnostic modality of choice in patients with stenosis. It is noninvasive and provides images in axial, coronal, and sagittal planes. MRI offers details of both the bony and soft tissue anatomy. It provides improved visualization of the soft tissue elements of the spine (Figs. 62-9 and 62-10). The degree of compression of the neural elements and the offending pathology are both easily visualized. The central canal, lateral recess, and neural foramen can all be visualized along with the degree of stenosis that is present in each of these regions. Facet arthropathy, ligamentum hypertrophy, disc bulges or herniations, and other compressive pathology such as synovial cysts are easily identified on MRI (Fig. 62-11). Foraminal stenosis is best visualized on T1-weighted sagittal images in which the nerve root and dorsal root ganglion are contrasted with the surrounding fat.
Overall, the diagnostic accuracy of MRI is similar to that of the CT-myelogram and does not have the drawbacks of ionizing radiation and contrast injection in the CSF. The reliability of MRI interpretation has also been investigated, and there appears to be significant inter-reader variability in assessing some anatomic locations. The measurement of thecal sac area, as well as the ratings of the degree of central and foraminal stenosis, show good reliability. The reading of the degree of lateral recess stenosis, on the other hand, shows significant variability. Although some have noted correlation between the degree of stenosis and outcomes of treatments, others have not been able to identify any such relationship.
It has been theorized that supine MRIs may understate the degree of stenosis because the patients may not be in the position of the worst compression during the study. Attempts have been made to demonstrate pathology in MRI scans that is obvious only under dynamic conditions. MRIs in flexion, extension, axial loading, and upright positions have been investigated without any conclusive evidence regarding their utility. It is unclear what the results of invasive treatments will be for those patients whose stenosis can only be detected under dynamic conditions. What the existing studies do point out is that the static images on the current MRIs should be supplemented with the dynamic information available from clinical presentation, as well as flexion and extension radiographs. One study noted that supine MRIs performed with the lumbar spine extended (by having the hips and knees extended) demonstrated more thecal sac compression than the images obtained in the flexed position. This suggests that position of the lower extremities during the MRI should be ascertained as a routine part of the patient's history.
Electromyography, Nerve Condition Studies, and Somatosensory Evoked Potentials
Electromyography (EMG), nerve conduction studies (NCSs), and somatosensory evoked potentials (SSEPs) are not part of the routine workup of patients with spinal stenosis. EMG identifies the effect of nerve function through recording the electrical activity of muscle at rest and with stimulation. EMG identifies lower motor neuron dysfunction and does not evaluate any sensory dysfunction. Electromyographic changes have been documented in up to 80% of patients with spinal stenosis. EMG can be useful in differentiating chronic changes from active ongoing denervation. However, it should be kept in mind that there is a significant incidence of false-negative electromyograms in patients with spinal stenosis. This can be attributed to the fact that EMG does not measure sensory dysfunction and thus does not catch the more common abnormality in patients with neurogenic claudication. EMG also does not help differentiate symptomatic from asymptomatic patients.
NCS measures the speed with which impulses travel down an axon. NCS is useful in differentiating changes that are occurring from neuropathy versus radiculopathy. SSEPs measure the electrical transmission of sensory stimulation starting from the peripheral nerves and going through the spinal cord and brain. A lesion in the peripheral nerve will prolong the latency response, whereas lesions of the root and cord will cause changes in the waveform. SSEP is more sensitive and specific compared with an EMG, although there continue to be false negatives and false positives.
Differential Diagnosis
Neurogenic claudication is the hallmark of spinal stenosis. Patients describe a variety of abnormal sensations that radiate down their legs with ambulation. Symptoms are typically relieved by forward flexion of the lumbar spine and are worse with extension. Sudden onset or severe motor weakness and bowel and bladder dysfunction in these patients should prompt evaluation of other etiologies of these symptoms such as cord compression. In spite of various attempts to create a single validated method of consistently diagnosing spinal stenosis, no single test or algorithm is available to accurately diagnose all patients with symptomatic spinal stenosis.
The differential diagnosis of spinal stenosis includes vascular claudication, lumbar spondylosis, lower extremity arthritis, cord compression, neurologic disorders, peripheral neuropathy, infection, tumors, and lumbosacral plexus lesions. Symptoms from neurogenic claudication start proximally and progress distally, whereas symptoms from vascular claudication start distally and progress proximally. Vascular claudication causes symptoms with a constant level of exertion regardless of the position of the lumbar spine. Thus leaning forward on a grocery cart or going uphill does not allow these patients to walk longer. Similarly, patients with vascular claudication continue to be limited on a bike, while the patients with neurogenic claudication have better endurance on a bike. On physical examination, painless full extension of the lumbar spine; shiny, hairless legs; and weak peripheral pulses are all hallmarks of vascular claudication.
Lumbar spondylosis typically causes pain in the low back without significant pain or abnormal sensation in the legs. Peripheral neuropathy typically causes burning pain and paresthesias that are unrelated to activity. A history of diabetes, vitamin deficiencies, alcoholism, chemotherapy, drug abuse, and exposure to toxins should be elicited in these patients. Physical examination in neuropathy patients will typically demonstrate hypoesthesia or dysesthesia in a glove and stocking distribution. Ankle reflexes will often be absent bilaterally. NCSs are helpful in establishing a diagnosis in these patients.
A history of isolated joint pain with ambulation will help identify patients with lower-extremity arthritis. Hip arthritis typically presents with groin pain radiating into the anterior thigh but can also be a cause of buttock pain. Physical examination demonstrating hip irritability and limitation in internal rotation suggests hip pathology is symptomatic. A thorough history and physical examination can thus help eliminate the majority of common conditions that mimic lumbar spinal stenosis. Presence of constitutional symptoms and intense nighttime pain suggest a possible infection or malignancy. These symptoms should trigger an MRI and laboratory studies, which would help eliminate these more rare conditions.
Summary
Lumbar spinal stenosis is a common finding in the elderly. With the aging population in the United States, the number of patients with spinal stenosis seeking treatment will dramatically increase over the next 20 to 30 years. Because pathologic changes can be present in asymptomatic patients, abnormalities found on imaging modalities are not a good method of diagnosing symptomatic spinal stenosis. Findings from a thorough history and physical examination should be correlated with corresponding pathologic abnormalities on MRI or a CT-myelogram. This is especially important if any invasive treatment will be recommended. Plain radiographs complement the other imaging modalities to create a full clinical picture that includes the detection of any dynamic instability. EMG, NCSs, and SSEPs are typically not helpful in confirming the diagnosis of stenosis. Despite our long history of treating patients with spinal stenosis, there is no single diagnostic test that can help identify patients with symptomatic spinal stenosis.
Pearls
- In patients with mild to moderate lumbar spinal stenosis, rapid or catastrophic neurologic deterioration is rare.
- Magnetic resonance imaging (MRI) is the noninvasive study of choice in patients suspected of having spinal stenosis.
- Imaging studies should be correlated with specific findings on history and physical examination that would be expected on the basis of the specific neural elements that are compressed.
- No single diagnostic test can confirm the presence of symptomatic spinal stenosis.
Pitfalls
- Abnormal imaging is not a reliable method of diagnosing symptomatic lumbar spinal stenosis. The incidence of clinically silent lumbar degenerative disease is high.
- Electrodiagnostic studies are not typically helpful in the diagnosis of spinal stenosis.
- Most patients with spinal stenosis have a normal neurologic examination.
- In evaluating patients with stenosis, do not forget to examine the hip joints and lower extremity vascularity.
Key Points
- Lumbar disc degeneration is a nearly universal finding in the aging population.
- Degeneration alone does not imply a pathologic entity. A disease may be said to exist relative to the symptoms with which the patient presents.
- In the absence of pathognomonic findings, the diagnosis of spinal stenosis rests on a Venn diagram approach in which historical elements overlap with physical examination and imaging findings.
- Once symptomatic, most patients will continue to have symptoms on at least an intermittent basis until surgically decompressed.
- On the other hand, rarely does stenosis progress rapidly. Therefore a trial of nonoperative management is indicated in most cases.
- Patients with symptomatic stenosis may present with one or more of a combination of axial pain, radiculopathy, and neurogenic claudication. Each of these is associated with different historical and examination findings.
Key References
- Weinstein JN, Tosteson TD, Lurie JD, et al.: Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 358:794-810 2008 PMID: 18287602 - A large prospective study evaluating outcomes of lumbar spinal stenosis patients treated with surgical versus nonsurgical treatment.
- Waters WC III, Baisden J, Gilbert TJ, et al.: Degenerative lumbar spinal stenosis: an evidence based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 8:305-310 2008 PMID: 18082461 - Evidence-based guidelines produced by North American Spine Society regarding diagnosis and treatment of patients with lumbar spinal stenosis.
- Atlas SJ, Keller RB, Wu YA, et al.: Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the Maine Lumbar Spine Study. Spine. 30:936-943 2005 PMID: 15834339 - A prospective observational cohort study evaluating outcomes of surgical and nonsurgical treatment after 8 to 10 years.
- Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, et al.: Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine. 3:319-328 1978 PMID: 741238 - A classic article describing the pathogenesis of lumbar stenosis.
- Verbiest H: A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 36:230-237 1954 PMID: 13163105 - A historical perspective on diagnosis and treatment of lumbar spinal stenosis.